MONDAY HEALTH BURST ON HEALTH IMPLICATIONS OF DRUG AND SUBSTANCE ABUSE
Drug abuse can lead to severe health issues that can be life-threatening. Here are some crucial points to consider:
Addiction: Those with addiction often suffer from health problems associated with lung or heart disease, stroke, cancer, or mental health conditions. (National Institute on Drug Abuse)
Mental health disorders: Drug abuse is linked to mental health issues such as depression, anxiety, psychosis, and an increased risk of suicide. Substance abuse can worsen existing mental health conditions or trigger new ones.
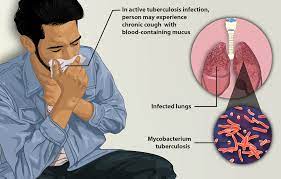
Physical health problems: Different drugs can cause various physical health issues. For instance, inhalants can damage the respiratory system, while stimulants can lead to heart problems and stroke. Additionally, injecting drugs raises the risk of infectious diseases like HIV and hepatitis.
Overdose: Drug abuse significantly increases the risk of overdosing, which can be fatal. This happens when an individual takes a toxic substance, leading to respiratory depression, organ failure, seizures, or coma. Opioids, like heroin or prescription painkillers, are primarily associated with overdose deaths.
Long-term organ damage: Prolonged drug abuse can damage vital organs such as the liver, heart, kidneys, and lungs. Chronic drug use may lead to liver cirrhosis, cardiovascular disease, kidney failure, and respiratory disorders.
Impaired cognitive function: Drug abuse can affect cognitive function, memory, attention, and decision-making abilities. Long-term drug use may cause irreversible damage to the brain’s structure and function.
In collaboration with Leap Africa, CFHI, in February 2023, educated more than 200 young people in Bwari local government, FCT, about drug and substance abuse, civic participation, and political thuggery. This was achieved through the Community Action against Drug Abuse project, funded by the MacArthur Foundation and the Ford Foundation.
It is crucial to seek prompt and appropriate treatment to address drug abuse and minimize its health consequences.
Monday Health Burst is an initiative of CFHI to address issues of basic health concern. Join us every Monday on all our social media platforms for more episodes.

MONDAY HEALTH BURST ON HEALTH IMPLICATIONS OF DRUG AND SUBSTANCE ABUSE Read More »